
But sometimes you just have to stand back and appreciate how science has allowed us to alleviate human suffering. I mean, I know most of us aren’t caring for kids with SCID – this study is not going to change my everyday practice. And they don’t require immunosuppressive medications either. None of the 48 kids required ADA injections again. Genetic labels attached to the new ADA gene were detected in all sorts of white blood cells – granulocytes, t-cells, b-cells. After treatment, it shot up.ĭeoxyadenosine – the toxic metabolite – plummeted. The average ADA level in their blood, before treatment, was close to zero. The average age of kids in this study was just under one year old. Two of the 50 kids did not have successful engraftment – both restarted enzyme replacement – one found a donor for a stem cell transplant.īut I want to focus on the 48 kids with successful engraftment. The modified cells are then reinfused, and, if all goes well, they take up residence in the bone marrow, start dividing, and give rise to immune cells that can metabolize all that deoxyadenosine. Meanwhile, the patient gets busulfan to knock down the number of wild-type stem cells in his or her bone marrow – essentially making room for the modified cells to engraft. The stem cells, now expressing ADA, are counted, evaluated for sterility and viability, and prepared for reinfusion. The virus has been modified so that it can no longer replicate, but includes the genetic machinery to change the RNA to it’s complementary DNA and to integrate that DNA strand into the nuclear DNA of the host cell. Outside of the body, they are exposed to a lentivirus vector which contains the ADA gene in RNA form. Now, a new report, again in the New England Journal, suggests that gene therapy for ADA-SCID is ready for the spotlight.įirst, stem cells are harvested from the bone marrow or peripheral blood. While this was no doubt a huge advance, a patient treated with this therapy subsequently developed t-cell leukemia, which may have been due to insertional oncogenesis – when the introduced gene gets stuck in the genome in a place that promotes cancer. The authors reported restoration of ADA levels in 8 out of 10 participants.

In 2009, the first report of truly successful gene therapy for ADA-SCID appeared in the New England Journal of Medicine. Gene therapy for ADA-SCID started in the mid 90’s, but had middling results – the altered cells didn’t live long enough in the body to provide much protection. Twice-weekly pegylated-ADA injections are considered a temporizing measure, but don’t seem to lead to as robust immune reconstitution as transplant does and can be prohibitively expensive.īut there is another option – gene therapy. But even matched transplants require lifelong immunosuppression, and only 20% of children with ADA-SCID find a match. Standard of care, these days, is stem cell transplant – ideally from a matched sibling. SCID evokes the image of the “bubble boy”.īut ADA-SCID does not require living in complete isolation anymore.
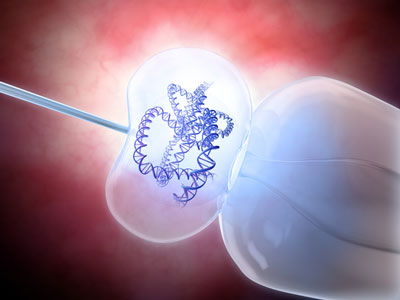
The conditions is known as ADA-severe combined immunodeficiency or SCID, and, untreated, most children born with ADA-SCID will die from infection before age 2. For most of them, the buildup of deoxyadenosine prevents their immune system from ever developing. So toxic, in fact, that if you couldn’t quickly break it down, those cells would die, leaving you exquisitely vulnerable to infection.įortunately, the chances are your DNA codes for a protein called adenosine deaminase which breaks deoxyadenosine down into more manageable substances.īut about 1 in 100,000 people are born with mutations in their ADA gene. Your body is producing it right now as a product of the breakdown of nucleic acids in your cells.


 0 kommentar(er)
0 kommentar(er)
